Health gets poor attention
Seventy-five-year-old Halima Begum has been undergoing treatment in Dhaka for the last three months as her eyes got damaged due to a stroke late last year.
A patient of hypertension and arthritis for around 20 years, Halima has been frequently visiting Dhaka for treatment as her sons could not rely on the doctors of their home district Natore.
“I am tired of visiting doctors and taking so much medicine. The doctors have recently said my kidneys have also got damaged for taking too much medicine,” she said.
She added her monthly cost for medicine is around Tk 1,500, while diagnosis requires almost a similar amount.
The health budget means a little to her. She rarely visited the Union Health and Family Welfare Centre, except for emergency or primary treatment, from where she was recommended treatment in Dhaka, not in upazila or district public hospitals that could provide healthcare at minimal cost.
Halima's story fits well with the country's health financing scenario where out of pocket (OOP) health expenditure is 63 percent of the total health expenditure, which is much higher than that of global average of 32 percent.
The OOP health expenditure pushes four to five million people into poverty every year, while many of the poor fail to afford minimum healthcare.
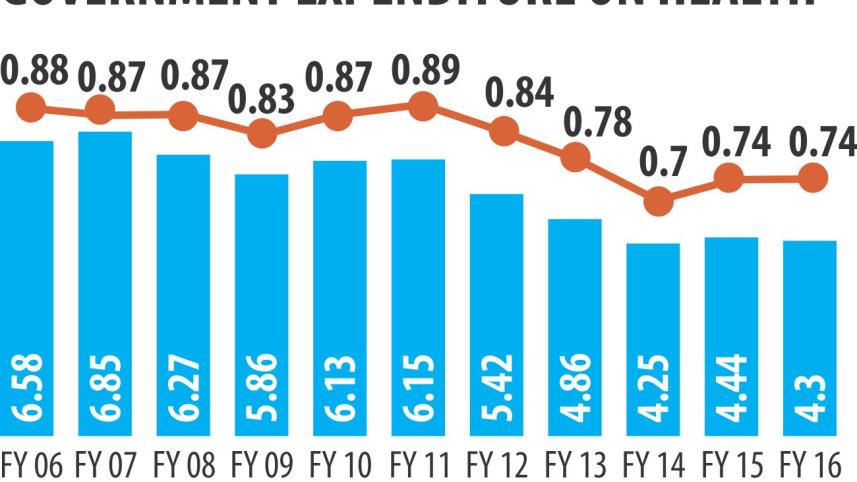
Yet, Bangladesh's proposed budget for health sector has declined.
For the next fiscal, it is Tk 17,487 crore, which, though Tk 2,676 crore more than that of present year, is lower by 0.47 percent as share of the total budget compared to present fiscal year's revised budget share of 5.6 percent.
This share is less than 1 percent of Bangladesh's GDP, while per capita total healthcare expenditure (THE) in Bangladesh is one of the lowest ($31.63), which is $255.94 in the middle income countries.
This declining trend continues when 33 percent under-five children are underweight and under-five child mortality rate is 46 per 1,000 live births and maternal mortality rate 170 per lakh live births.
“Our major health challenges now are non-communicable diseases and out of pocket health expenditure,” said Dr Hossain Zillur Rahman, executive director of Power and Participation Research Centre (PPRC).
Of the 8.86 lakh deaths that occurred in Bangladesh in 2012, 59 percent were caused by non-communicable diseases (NCDs), including cancer, chronic respiratory diseases, diabetes and others, while 9 percent by injuries, according to a WHO study released in 2015.
The budget proposes to add 235 more community clinics to the existing 13,126 in rural areas, expanding telemedicine but nothing about addressing the rising NCDs with the rising aging population.
Dr Hossain Zillur said preventive measures are now more important than curative ones. It requires better health education, safe food, food habit, hygiene and sanitation that need more allocation.
The issues of preventive measures involve several ministries like LGRD, food and agriculture and water resources, but the health ministry has to take a policy leadership. Such leadership role is not present, he noted.
Interestingly, when preventive measures should get more focus, the budget proposes withdrawal of VAT exemption on meditation service that is a natural way of mental and physical wellbeing.
Earlier, meditation service was exempted of 7.5 percent VAT in 2013-14.
In the urban areas, there are no adequate public health facilities that are in place at union, upazila and district levels in rural areas. The urban people, especially the poor, directly go to the specialised hospitals like Dhaka Medical College Hospital for primary care.
“If there was a hospital for primary care at ward levels, tertiary level hospitals would not be crowded. In that case, they could better serve the critical patients,” he said, suggesting more investment for urban healthcare facilities. According to Bangladesh National Health Accounts, 65 percent of OOP health expenditure is spent to buy medicines.
“The government should immediately intervene to expand the list of essential medicines and ensure their supplies free of cost,” Dr Hossain Zillur said.
Prof Syed Masud Ahmed, director, centre of excellence for Universal Health Coverage at Brac University, suggests allocating more funds to ensure presence of health personnel in rural public facilities by creating an enabling environment.
He believes if primary and mid-level diseases can be treated at local levels, rural people would not need to go to city hospitals except for severe illness. This would cut OOP and improve healthcare quality.
He suggests higher allocation to address the health issues for those living in the remote areas and marginal groups.




 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel.
Comments